Unlocking the Full Potential of Remote Patient Monitoring: Why True EHR Integration is Key to Scaling RPM Programs

Remote Patient Monitoring (RPM) has shown great potential for improving the health of individuals, and yet, by-and-large, it has failed to take off. Most RPM programs fall far short of scaling to the point of making a real impact. A big reason RPM programs tend not to take off is lack of true EHR integration, and treating it as an isolated intervention, instead of a key layer of insight over traditional care delivery.
Picture it: a physician’s office, 6:02pm. You’re a clinician who’s been trying to pilot a new RPM solution and are now juggling more systems than ever; one for receiving alerts about patient vitals, another for reviewing your patient panel at a population level, and of course, an overflowing secure message inbox alongside your EHR where you have to finally document all your decisions, sign orders, and hopefully pull the full patient picture together. You’re copy/pasting data between systems like it’s 1999. Every time you get an alert about a patient’s blood pressure spiking in one system, you have to manually log into another system to do anything about it. And this is just for the 20 patients in your pilot! Now imagine scaling that across hundreds of patients. That’s burnout waiting to happen, so most of the time after an initial trial, the login to the outside RPM portal is quickly forgotten.
It doesn’t have to be this way. With true EHR integration, all patient-generated data is right where it should be; embedded in the clinician’s workflow, right in the EHR itself. And that makes all the difference in scaling RPM programs. Here’s why.
What Is True EHR Integration?
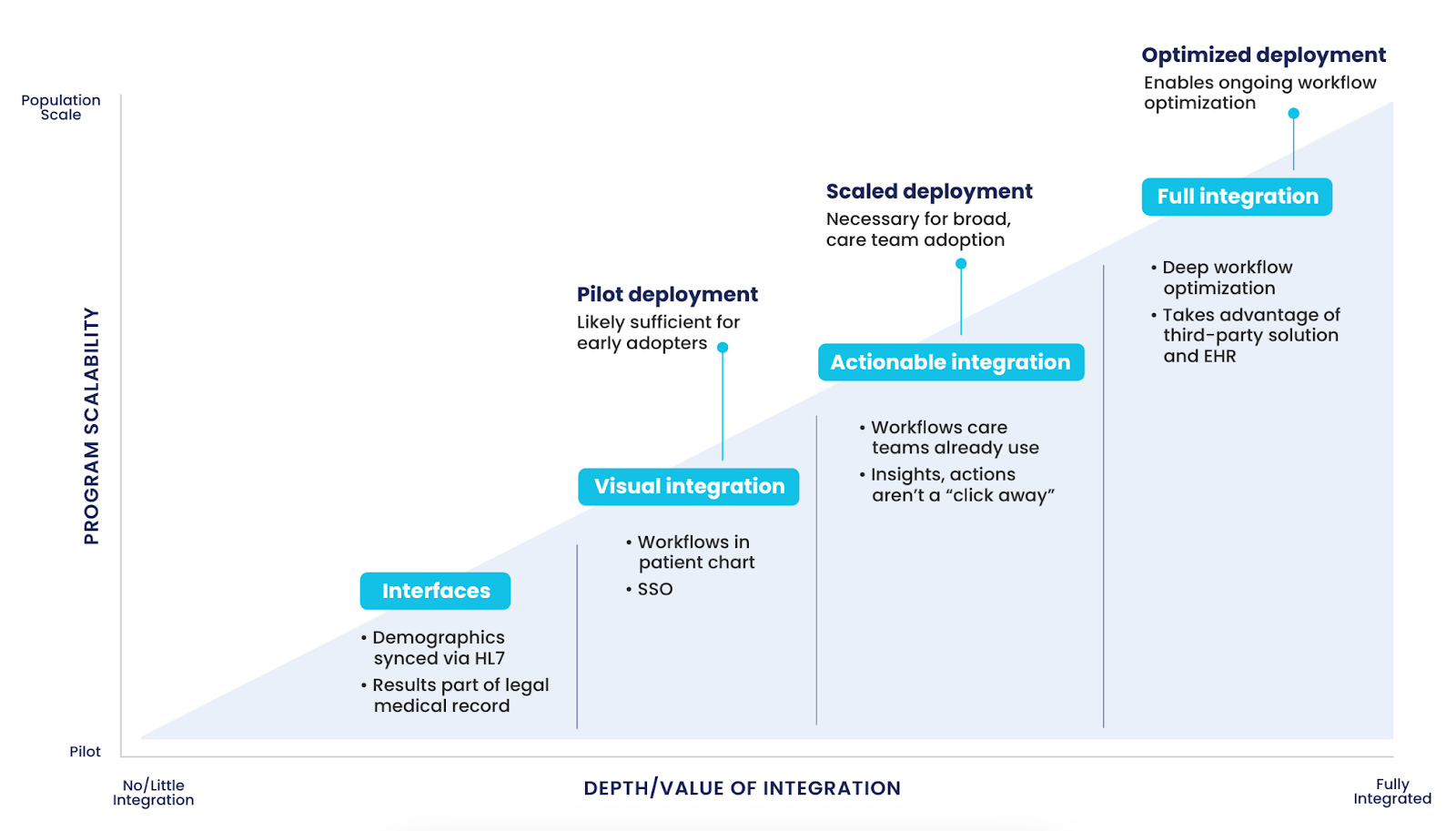
There’s a big difference between having an RPM solution that can “talk” to the EHR (interfaces) and a digital care solution that’s actually integrated into it. A lot of solutions can send over reports, download PDFs, or exchange HL7 messages. That’s part of the answer, but it’s not real integration.
True integration means the RPM platform isn’t a separate system you have to log into. Instead, it’s baked directly into the EHR, working as part of the same toolkit clinicians are already using. From notifications and data trends to patient histories and discrete data, everything is visualized and actionable right inside the EHR workflow.
This is where solutions like Validic come into play. With its integration into Epic and Oracle Health, for example, patient data flows seamlessly into the provider’s EHR; no need for extra logins and no extra hassle. Notifications flow into the provider messaging toolkit (InBasket, Message Center, etc), and clinicians see what’s going on with their patients without leaving the EHR. Flowsheet trends too hard to decipher? Purpose-made visualizations are right there in the chart too. Even better, every member of the care team who has access to the patient’s chart has access to the RPM data, so there’s no extra sign-ins, no extra admin tools to manage access to, and no extra steps to get someone set up to cover for you when you’re on vacation.
Why Does This Matter for RPM?
True EHR integration fixes major issues that plague RPM programs trying to scale.
1. Workflow Efficiency
Clinician burnout is real. Studies have shown that up to 63% of physicians experience some form of burnout, and a big chunk of that comes from disconnected workflows, disparate systems, and extra admin work. When your RPM platform is separate from your EHR, you’re asking doctors and nurses to do more; remember to log into another system, remember another password, and copy/paste, screenshot, or manually import data into the EHR. Not only is this extra administrative time documenting, separate passwords and logins leads to, let’s be honest, just not using the system.
When RPM is integrated directly into the EHR, these problems disappear. The data and insights are just there. No more switching between systems or double-checking that you entered the right numbers. Instead of fighting with technology, clinicians can focus on patient care, which is where their attention should be.
2. Increased Data Accessibility and Actionability
When RPM data is siloed in a separate system, it loses a lot of its value. If clinicians can’t easily access or act on the data, what’s the point? True EHR integration ensures that RPM data is immediately accessible, but more importantly, it’s actionable.
With a platform like Validic, all that useful patient-generated data, whether it’s glucose levels, blood pressure readings, oxygen saturation, qualitative feedback from surveys, or trend observations is not only visible in the EHR, but it’s presented in a way that lets clinicians act on it. Notifications are sent in near real-time, and clinicians can set custom notifications for at-risk patients. If a patient’s readings go out of range, the system flags it, and the care team can intervene before things get worse right there in their clinical workflows, easily including the relevant background in their clinical notes.
3. Enhanced Clinical Decision-Making
Truly integrated RPM facilitates easy clinical decision-making. With a steady stream of real-time patient data, clinicians can catch trends early. Is a patient’s blood pressure creeping up over time? Are they not adhering to their medication regimen? It’s not just about RPM data existing in the EHR, it’s about how it’s presented. True integration allows clinicians to spot trends within the context of the patient's entire medical history, all in one place, not isolated on a separate web portal dashboard. They don’t have to piece together the puzzle from different systems; the data’s already connected.
Scaling RPM the Right Way
Scaling RPM to large populations isn’t easy, but true EHR integration is the key to making it possible. Let’s take Kaiser Permanente, one of the largest healthcare providers in the U.S., as an example. Kaiser Permanente wanted to roll out RPM across its massive network, but that wasn’t going to happen with a disjointed system. They needed an RPM solution that could scale across regions, while fitting neatly into their existing clinical workflows. And that’s exactly what they achieved with Validic.
With True EHR integration, Kaiser Permanente’s clinicians didn’t have to change the way they worked to accommodate RPM. The system just fits. The result? Kaiser Permanente could efficiently monitor a growing number of patients with chronic conditions, across multiple regions, all while using their existing EHR as the central hub of information.
Scaling RPM is about more than just adding more patients; it’s about making sure the technology can handle increasing volume without overwhelming clinicians or IT teams. That’s why having a platform that integrates directly into the EHR, streamlines workflows, and requires minimal IT intervention is essential for long-term success.
The Real-World Impact of True EHR Integration
This isn’t just theoretical. Validic’s integration into Epic and other EHR systems has led to real, measurable improvements for healthcare organizations across the board. For one, the implementation process is streamlined. Validic clients have been up-and-running with patient enrollments days after the technical implementation is complete, and one Validic client reported patient check-in times decreasing from 15 minutes to 5.5 minutes once they implemented Validic. Because True EHR integration takes advantage of all the organization’s existing investments in EHR and workflow configurations, the technical work and training are much less than a typical implementation.
Beyond that, patients are seeing better outcomes. With more consistent monitoring and earlier intervention, healthcare providers can prevent complications and hospitalizations before they happen. RPM becomes proactive rather than reactive.
Get It Right with True EHR Integration
If you’re looking to scale your RPM program, the solution isn’t more devices or better alerts (though Validic supports more than 580 devices and has amazingly sophisticated notification rule capabilities)—it’s true integration with your EHR. Without it, you will be creating more work for your clinicians, risking burnout, and missing out on the full potential of RPM.
So, stop thinking of RPM as a standalone solution. Make it part of your clinical workflow and part of your EHR. Your care teams (and your patients) will thank you.
Interested in learning more about how to achieve this? Drop us a line at hello@validic.com. Validic has you covered, with a platform that not only integrates directly with your EHR but also supports over 580 apps and devices, all through a single integration point. The future of healthcare is here—let’s make it seamless.