The leading Connected Health Data platform and EHR-integrated solution for remote care
Validic empowers health systems, health plans and VBC organizations and applications with seamless Patient Generated Health Data integration to drive superior outcomes, and personalized care at scale.
Validic empowers health systems, health plans and VBC organizations and applications with seamless Patient Generated Health Data integration to drive superior outcomes, and personalized care at scale.
For Providers
Health systems and provider organizations
Remote care that works inside your EHR, not around it.
For Value-Based Care
Improve risk contract performance
Close gaps. Prevent admissions. Hit your targets. This is how VBC organizations turn risk into ROI.
For Health Plans
Engage Members With Purpose
Harness remote patient-generated data for engaging, outcome-driven member programs.
The ONLY solution that flexes with your needs.
From our developer-friendly Health IoT platform to our award-winning, fully EHR-integrated personalized care solution, Validic is the standard for making personal data actionable.
It all starts with our health IoT platform, healthcare's first and largest streaming platform for personal health data. We help you manage and access your population's health data - ensuring you trigger the right insights to support the right actions.
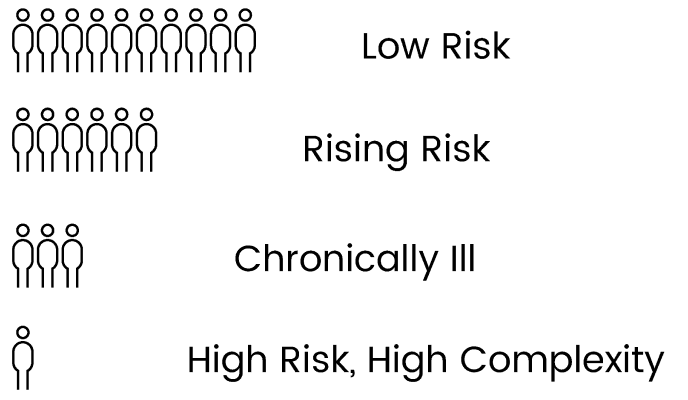
Our platform puts patients and providers “on the same page” with what’s happening day-to-day. Use patient-generated health data collected and transmitted automatically to the EHR to make informed clinical decisions, together. Spend time with patients who need a high-touch approach, while staying informed and connected to those who don’t.

.svg?sfvrsn=beacd7b5_1)