Remote patient monitoring has failed -- now what?

A health system telehealth leader recently told me they have been running a remote patient monitoring (RPM) program for the last couple of years, and things are “going well.”
“People are signing up for the program, and we are seeing good clinical results.” Long pause. “But…we want to extend this to other use cases, and our vendor is limited in the programs they can support. We also want to bring RPM to other areas of our health system but it’s too expensive.”
If the above sounds familiar, then it’s likely that you, like many of us, have been excited by the promise of RPM but disappointed by the reality.
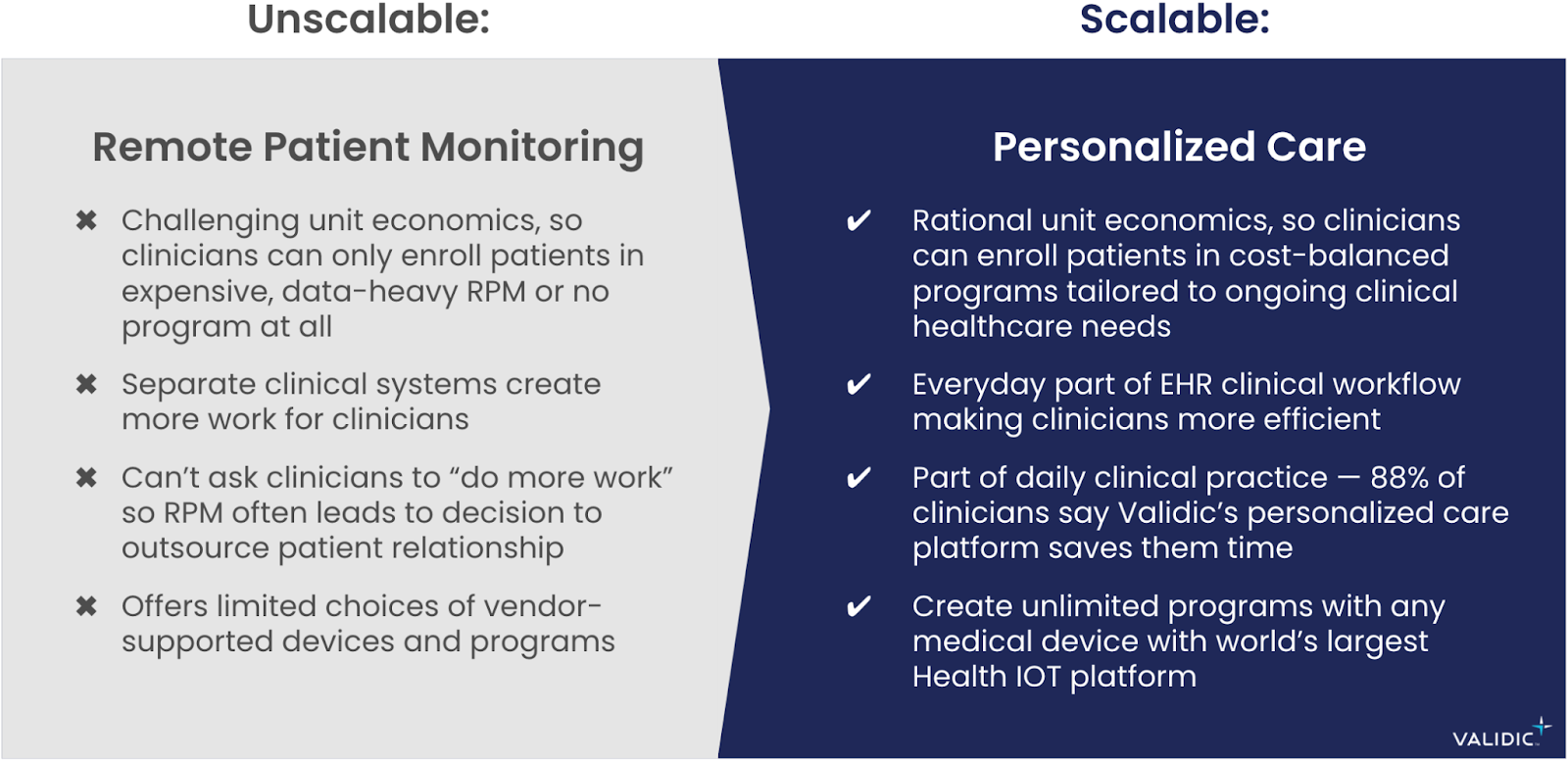
The business model of remote patient monitoring has failed.
The promise and failure of RPM
120 million U.S. adults are living with a chronic condition, including four out of five U.S. seniors (and an ever-aging population). Meanwhile, 47% of healthcare workers are planning to leave their position by 2025. With fewer practicing clinicians, and more people who need more care, technology augmentation is critical.
RPM promises to help clinicians improve clinical outcomes for more patients while lowering the total cost of care. Yet the vast majority of RPM deployments are stuck in the small pilot phase. These 50- or 100-person pilots are not going to help our overburdened clinicians meet the needs of a growing and aging patient population.
In fact, if a healthcare organization only cared about improving clinical outcomes for these 50 patients, it wouldn’t need RPM. It would be more cost-effective and less operationally disruptive to have a nurse practitioner call each patient and spend 15 minutes on the phone with them every other week. Presumably, the patients would improve, and love the one-on-one attention.
But 50-patient programs are not the goal and will not address growing patient demand. So why are most healthcare organizations stuck in “RPM pilot mode?” To answer this, we interviewed hundreds of health system executives and asked them one simple question: Why don’t you use RPM with all your patients?
The responses can be summed up, in aggregate, as:
We want to scale RPM because patients love it, and the clinical results are good. At scale, it should help our clinicians streamline their work. But RPM is really expensive. When it works, people are healthier, which creates fewer billable events. We don’t need these programs to be wildly profitable, but we can’t lose money on them.
In short, RPM isn’t expanding beyond small pilots because healthcare organizations can’t find a path to break even on the investment. The cost structure is too high.
Pilot programs lead to poor tradeoffs
When running RPM pilot programs with small numbers of patients, program managers often overlook key features important for scale. One of these “tolerable” tradeoffs is working in web-based clinician portals instead of an EHR workflow-integrated solution. This seems acceptable because EHR integration requires IT time and buy-in, whereas organizations can deploy web-based solutions quickly.
However, as a clinician wraps up their workday, will they be finishing up clinic notes for patients they saw, or logging in to an external tool to check on patients they haven’t heard from? (Validic can deploy embedded in the EHR or as a web portal and we will tell you, clinicians always prefer to stay in the EHR.)
RPM pilot programs typically use web-based portals, so healthcare organizations often come to the conclusion that while RPM is clinically effective, it creates “yet another thing to do” for clinicians. And with today’s workforce crisis, we absolutely cannot ask clinicians to do more work.
Because web-based RPM solutions create more work for clinicians, healthcare organizations sometimes decide to outsource the RPM clinical management. In other words, the RPM solution that created “one more thing” for clinicians to do is now asked to outsource a healthcare organization’s core clinical competency and valuable patient relationships.
Outsourced clinical services are even more expensive and further remove healthcare organizations from evolving how they deliver patient care. As an example, a health system executive recently told me they are using a RPM vendor with outsourced clinical management to monitor a small number of complex high-risk patients. When the health system identifies a patient for the program, the vendor enrolls and monitors the patient for two months. I asked the executive what they do with the patient after two months: “Nothing, we unenroll them. The RPM program is too expensive, and it’s all we can afford.”
There is an alternative to these endless and likely frustrating RPM pilots — one that saves clinicians time and helps healthcare organizations cost-effectively deliver better care for their patients.
The solution is personalized care
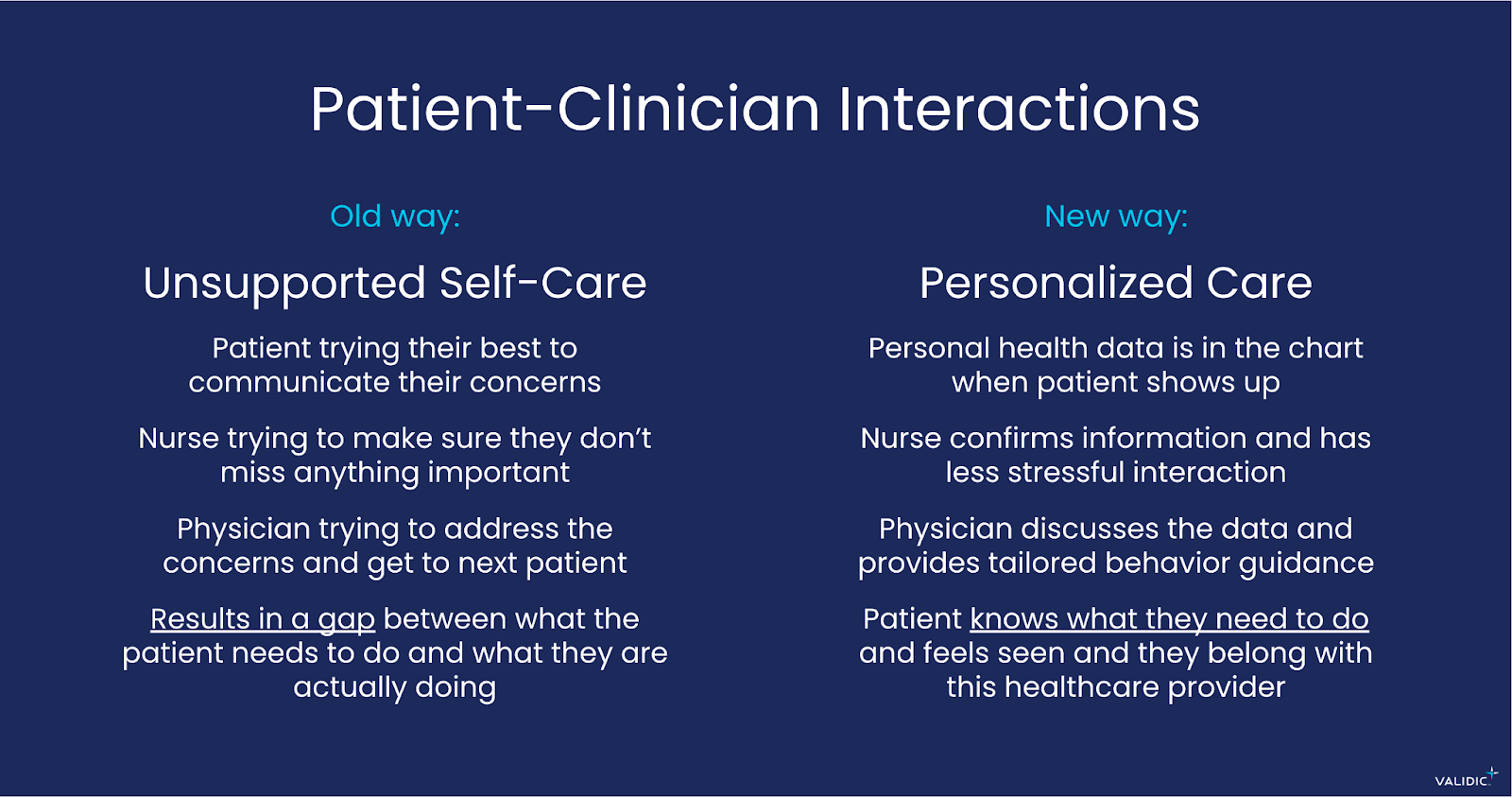
We all know that the health data gathered during a routine office visit offers only a point-in-time snapshot. And while important, it provides an incomplete picture of overall health and doesn’t accurately reflect everything that is happening in a person’s life that could be impacting their health and well-being. These brief office visits and episodic health data provide little context for clinicians and often lead to well-intentioned but generic advice, like: “You need to eat a healthy diet and walk more. Here’s a printout of information to help you get started.” This typical interaction is why 76% of patients are frustrated when leaving their medical appointments.
With personalized care, clinicians can view patients’ everyday data in the patient chart. This way, when the patient calls or comes in for an appointment, clinicians have relevant, timely data available in the patient chart. Clinicians now have the context they need for a shorter, more personalized patient interaction.
As one executive director of virtual care with whom we work put it: “People are not a disease. They can’t be defined by a single condition. With Validic, we can look at people holistically within the context of their own ‘normal.’” Personalized care is what clinicians aim to deliver every day, but they lack modern tools to do so effectively.
A study looking at Validic’s personalized care solution found a 63% decrease in the amount of time clinicians spend on the phone with patients enrolled in the programs (from 15 minutes down to 5.5 minutes on average). In a client survey, 88% of clinicians responded that the personalized care solution saves them time, and 92% said they feel like they are delivering better care.
These results are because personalized care takes everyday patient data and integrates it as a first-class citizen of the EHR. Clinicians don’t see this as “yet another thing to do.” Quite the opposite: they see it as a valuable productivity tool that helps them deliver better care in less time.
Personalized care is the future of remote care
In the late 1990s, dozens of upstart technology companies created video phones, seeing that the internet would unlock this more personal communication. These devices languished and never took off because they were expensive, and didn’t integrate with people’s daily lives. Today, we all have a video phone in our pocket. But it’s just one feature integrated with a device that we use every day.
Traditional remote patient monitoring companies are like those old video phones. They have the right idea, but health systems will never scale until the programs are cost effective, and clinicians will never adopt the technology until it is a seamless part of their daily workflow.
We can make good on the promise of remote care technologies to improve quality, lower the total cost of care, and help clinicians operate more efficiently. For example, Validic’s solution supports the largest personalized care program in the U.S. at Kaiser Permanente. More than 7,000 clinicians across seven regions have enrolled more than 300,000 patients with chronic and acute conditions. The success of this program is owed to the fact that the technology is a part of their Epic EHR clinical workflow. It is easy for clinicians to adopt, and patients love the programs.
With more people needing more care, and fewer healthcare workers available, we need smart, workflow-integrated, tech-enabled solutions that allow clinicians to practice at the top of their license and operate more efficiently.
Clinicians do not practice remote patient monitoring. They practice personalized care. Let us introduce you to the first EHR-integrated personalized care solution that helps your clinicians deliver better care, in less time, while creating more meaningful patient experiences.