Launching a successful remote patient data program
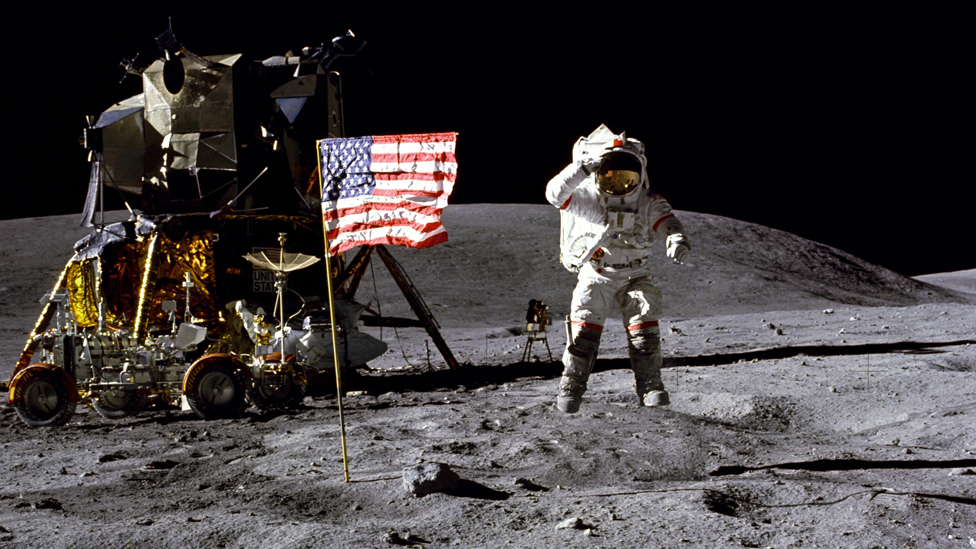
A note from the author: I’m a space and sci-fi nerd, so before we begin I’ll ask you, dear reader, to forgive the overly-abused metaphor that will hold this blog post together.
“Three….Two….One….Liftoff” are the words teams at space agencies spend years laboring to hear. The culmination of meticulous design, engineering, planning, and testing, liftoff is the nail-biter moment where you find out if the planning was enough. Got something wrong six months ago in the engineering stage, or did the math wrong on the temperature tolerances of a single component? Tragedy.
Fortunately, launching a remote patient data program doesn’t come with the same hard line between pre-liftoff and post-liftoff. Selecting a remote patient data solution that takes a platform-first approach enables teams to continually adjust design and workflow, swap in new devices and program parameters, and make real-time decisions about their program based on real-world insights.
Despite this, it is fairly common in large organizations to iterate and iterate on ideas and design pre-launch; bringing in new stakeholders, theorizing different strategies, and generally over-complicating “phase 1.” Much of this is understandable; if phase 1 requires a lot of fuel (time, effort, political capital, money) to launch, we want to make sure the payload that gets delivered into orbit is perfect.
What if there was a different way? What if, instead of riding a very expensive, very dangerous controlled explosion into space over the course of 2-3 minutes, people and payloads could comfortably ride a well-established elevator up to orbit over the course of several hours? It sounds like science fiction, but there are real scientists and engineers working on the concept of an orbital lift; a cable that runs from the surface of the Earth to an orbiting anchor. In this system, very little energy is expended for each ride up to orbit, and it’s an incremental journey that is far safer.
At Validic, we’ve seen both of these implementation strategies play out numerous times with remote patient data projects. The traits we see in the most successful programs include:
Executive champion
Every space mission has a flight director. While there are many moving parts, ultimately someone has to make the hard decisions and herd the cats along with them. Without fail, every successful program we have seen has a clearly-identified executive champion who is empowered to make decisions.
This person in the successful programs we have seen are typically the CMIO of the organization or a digital health executive charged with the overall digital patient experience. Much of this alignment is based on the key driver for the program.
Is it for more high-risk patients where the organization is working to drive down readmissions and inpatient utilization? Alignment to the CMO or CMIO makes a lot of sense in this case. Is it to help drive efficiency for primary care and specialists, along with their nursing staff? In this case, the CMIO or CNO are strong drivers for those needs.
Improved patient experience, satisfaction, and “stickiness” are key drivers for the chief marketing officer. If the organization has tapped a chief digital officer role, this role can be the unifying force across all of these functions.
Regardless, because remote patient data is a fairly new strategy to most organizations, it’s typical that budgets, decision-making paths, and even “what defines success” will not be established. Identifying a “flight director” who can work on these things directly with their remote patient data solutions partner is critical.
Clear, but flexible, mission parameters
On September 12, 1962, President John F. Kennedy announced that we would send a rocket to the moon and return it, and its crew, safely back to earth. Bold? Yes. Audacious? Absolutely. Unclear about the goal? Nope. The mission parameters were clear and simple. Get to the moon, come back safely, and do it before the clock strikes midnight on the night of December 31, 1969.
Imagine if JFK’s speech said “today we’re committing to doing more space stuff.” Similarly, we have seen multiple examples of remote patient data programs that started with unclear mission parameters fail to launch. At the same time, we have seen programs that have very clear mission parameters surprise and exceed both the expectations of their executive sponsors and their original program goals.
Strong starting points for remote patient data programs that we have seen include:
- Digitize the paper logbook and automate the capture of home blood glucose and blood pressure values for all of our newly-diagnosed diabetics and hypertensives to improve the efficiency and adherence to standards of care for our primary care and endocrinology practices.
- Numerous organizations have begun remote patient data programs with the first use case being to intercept patients with declining health status after a recent heart failure discharge to avoid unreimbursed readmissions.
- A community health group on the east coast launched a program to monitor hypertension in their largely urban, sometimes transient population, quickly ramping up to more than 1,000 patients enrolled in the program by staying focused on a specific goal of monitoring home blood pressure values in a scalable way.
Once a starting point has been identified, decision-making in the early stages of a program becomes much clearer and straightforward.
Solutions that are laser-focused on a single condition or high-touch interventions perform extremely well during smaller pilots, but introduce challenges when organizations start trying to scale to additional use cases and orders of magnitude more clinical users.
A flexible platform
Though the program had other challenges, the Space Shuttle was the NASA workhorse for 30 years for a variety of missions because of its flexibility. It helped assemble the International Space Station, conducted scientific missions in space, delivered commercial satellites to orbit, launched deep space probes, deployed and serviced space telescopes, and provided a habitable living space for American space explorers. Its flexibility and configurability for different missions is what enabled the same platform to be used for three decades.
Successful remote patient data programs should start with solutions that are flexible and will enable them to more readily adapt the solution to future use cases. Even with fairly streamlined launch projects, the process of vendor selection, procurement, implementation, and integration to onboard a new vendor partner requires a lot of time and investment. Making those investments for individual solutions supporting single, small programs is not sustainable for an organization long-term.
Solutions that are laser-focused on a single condition or high-touch interventions perform extremely well during smaller pilots, but introduce challenges when organizations start trying to scale to additional use cases and orders of magnitude more clinical users. Solutions that are designed to be used as a stand-alone “mini-EHR” do not do well beyond pilots when EHR integration moves from a nice-to-have to a #1 necessity.
Redefining pilot
In the IT world, it has been long-debated whether “big bang” deployments are better or worse than incremental, phased deployments. In our experience, we have seen the most success come from organizations that think differently about how to “pilot” remote patient data. Rather than rolling a lot of stuff out to a small group, they roll out a small amount of useful stuff to a lot of groups.
For example, instead of launching a stand-alone RPM kit for 2 providers and 50 patients, they roll out a lighter-weight, lower-cost program to dozens or hundreds of clinicians. This approach starts with an immediate improvement on a thing those clinicians are already dealing with, like simply “turning on the button” to enable providers to invite their diabetics to share their self-measured blood glucose values so they’re teed up at the next visit. Once visit prep has become streamlined, then providers will be better poised to decide who they’d like to have alerts set up for and who they might want to provide a kit.
In this way, because both the cost and risk are lower in these kinds of programs, a program can launch faster and broader, enabling a lot more providers to try it out and then evolve along the way, rather than trying to get the complex program perfected before launch.
In summary, just like a successful space program, having a clear “why” to start the project and build enthusiasm, a defined decision maker who can make the tough calls, a first phase that goes broad instead of deep, and selecting a flexible platform that can evolve with your program’s sophistication and learnings over time are some of the main things our most successful clients have in common.
If you’d like to learn more, or talk with one of our experts, please reach out to Validic at hello@validic.com. If you’d like to talk about these ideas or space exploration, please reach out to me directly at brian@validic.com.