Episodic care model is failing 100 million Americans living with chronic conditions

My grandmother, Betty, was the center of my dad’s family. She was infinitely kind, raised seven children in a small town in Iowa, and later in life managed an always rotating cast of visiting family members. She made sure meals and snacks were on the table each day, “at 7, 11, 3, and 7.” If you were at my grandma’s house and didn’t show up at those times, you didn’t eat.
Caring for others meant that my grandma unfortunately didn’t take care of herself. She was a lifelong smoker, she didn’t exercise, and she cooked and ate a farmer’s diet. Later in life, alongside obesity and hypertension, my grandmother was diagnosed with COPD. It was this last condition that unfortunately ended her life. She was in her room at an assisted living facility when her lungs gave out, and she passed out before she was able to call for help. She never woke up.
There are millions of Bettys out there. 129 million U.S. adults are living with a chronic condition, including 4 out of 5 U.S. seniors. We in healthcare see these as population health statistics. But they are more than that — these are real life moms, dads, brothers, sisters, uncles, aunts, cousins, and friends.
The most difficult part for me about my grandmother’s death is that it, while ultimately inevitable, was preventable. My grandmother had been discharged from the hospital due to complications with her COPD less than 48 hours before. A study of over 1.2 million people hospitalized with COPD found a mortality rate of 26.2% in the first year. The same study found that interventions that extend beyond the first month after discharge may be needed to improve longitudinal outcomes. My grandmother was returned to her assisted living facility with no continuous monitoring intervention. She is now a statistic.
We saw the positive impact of remote monitoring programs during the height of the COVID-19 pandemic, and there is evidence that continuous care yields improved health outcomes for people living with chronic conditions. Yet, we approach chronic condition management like we do acute, episodic care. We wait until people are acutely sick, treating the symptoms of a chronic condition rather than addressing the underlying behaviors that exacerbate and progress the condition.
It is not only people like my grandmother, and their families, who are losing out on improved quality of life due to healthcare’s focus on acute, episodic care. Our entire country is losing. A 2021 report by the Commonwealth Fund compared the United States healthcare system against 10 other high-income countries. Despite spending more per capita on healthcare, the study found “the U.S. ranks last on access to care, administrative efficiency, equity, and healthcare outcomes, but second on measures of care process.” It is shocking how a country as wealthy as ours and seemingly driven by patriotism could allow this to happen. We are dead last (pun, unfortunately, intended).
Yet even when people seek care earlier for chronic conditions or pre-chronic conditions and doctors put care plans in place, there is usually only so much a physician can do based on the information and data available.
Episodic care doesn’t work for chronic conditions
Provider-generated health data only offers a point-in-time snapshot. This data is vitally important, but provides an incomplete picture of overall health and doesn’t accurately reflect everything that is really happening with a person’s life. It’s like trying to understand the plot of a movie through a series of random screenshots.
Here is a visual representation of provider-generated health data:
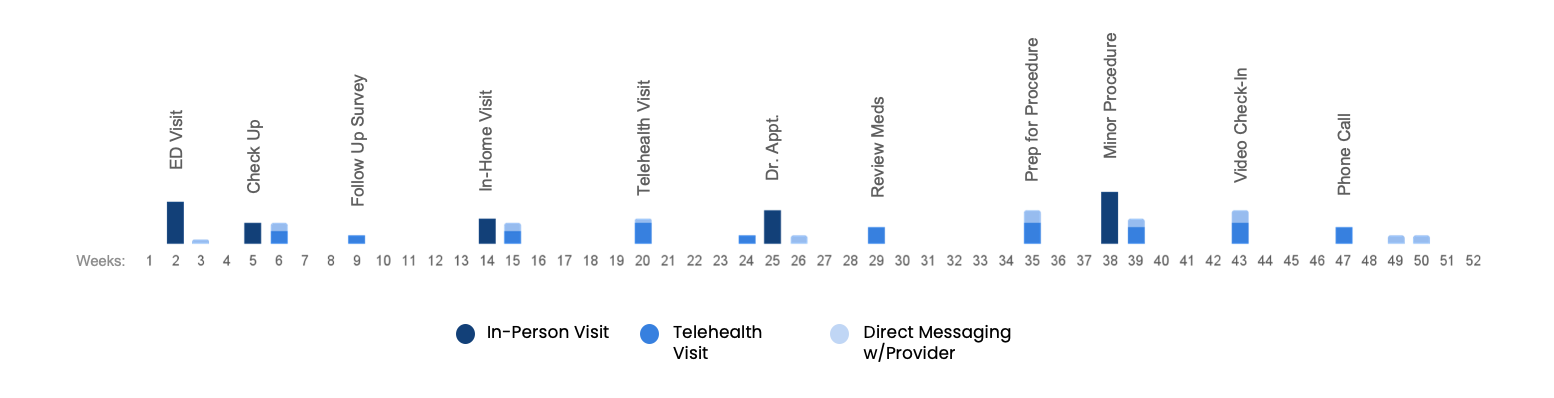
Figure 1. Provider-generated health data
Conversely, the personal data we generate every day matters the most to our health. It is this rich personal health data that can drive intelligent, cost-effective clinical care, especially for those living with chronic conditions. Yet, this data is often used the least when providing healthcare.
Here is a visual representation of the richness of personal health data:
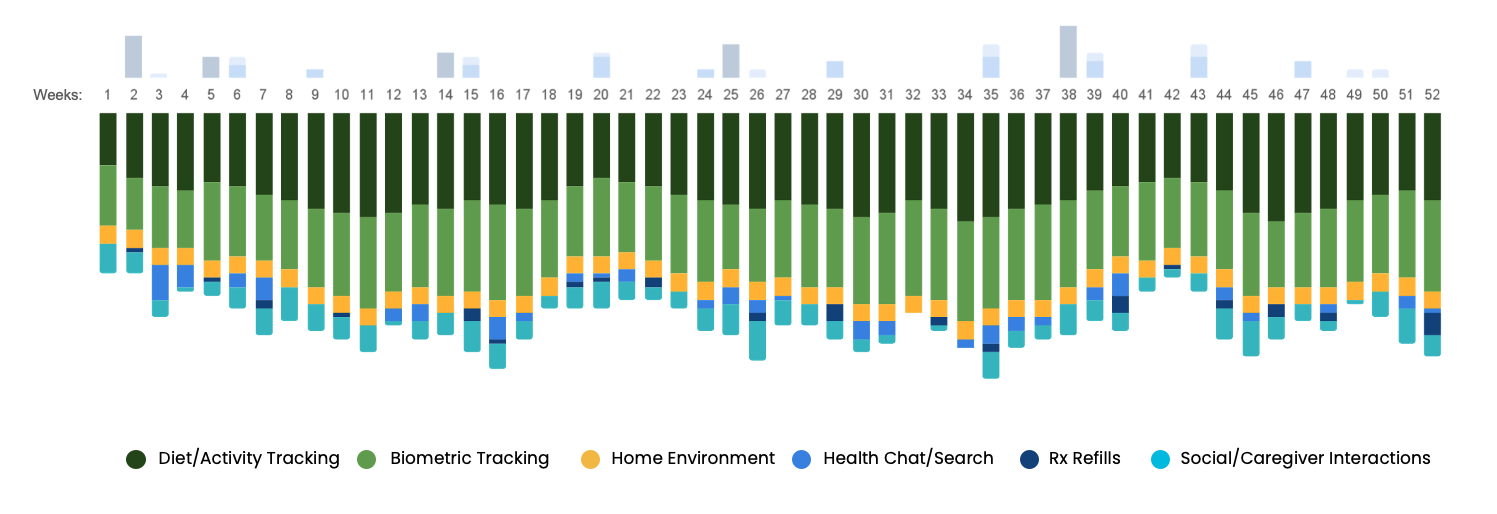
Figure 2. Consumer-generated health data
Bringing parity to personal health data
This is a lot of data, and we can’t ask healthcare providers to “do more” or sift through mountains of information. Instead, we need to make personal health data a “first-class citizen” of the electronic health record (EHR) through clinical workflow integration. With this workflow integration, physicians and care teams can interpret and use personal health data in the same way they use clinical data – to inform, diagnose, treat, and have meaningful conversations with patients about the data, and adjust care plans accordingly.
For example, when a physician orders a fasting blood glucose test for a suspected pre-diabetic patient, they generate the order from within the patient’s EHR record. After the lab processes the result, the physician receives an alert within the EHR message center saying a result is ready to view. They view the result within the patient’s chart. Then, when the patient comes into the office for a follow-up appointment, the physician has a conversation with the patient about what fasting blood glucose means and can reference the lab result as part of that conversation.
This is how Validic clients use personal health data to triage, diagnose, and treat patients. The workflow is identical and includes patient-generated health data from devices used in a patient’s home or other remote locations. If a physician wants to incorporate daily blood glucose readings into a patient’s care plan, they can prescribe a diabetes remote care program from within the EHR. The patient begins taking readings with a connected glucometer and the readings are transmitted in real time through Validic’s health IoT platform and displayed in the patient’s medical record. The physician receives an alert when the system flags the reading as out of range or needing attention. The next time the patient has an in-office or telehealth visit, the data is available within the patient’s record for the physician to reference during the conversation.
Consumers are in the driver’s seat
Virtual care is here to stay and consumers now demand the same flexibility, accessibility, and ease of use for their healthcare experience as they do with other experiences like online shopping and banking. Additionally, use of connected devices to manage health and wellness continues to increase, and the desire is there to incorporate these devices and data into healthcare delivery to drive meaningful change and outcomes improvement.
In a recent Deloitte survey, one-third of smartphone users said they monitor their health or track their fitness with their phones. Nine out of 10 consumers use wearables to track common health and fitness metrics like daily steps, pulse rate, health and nutrition, heart health (ECG), blood oxygen (SPO2), and sleep quality. And seven in 10 of consumers feel these devices have improved their health.
It is both painful and heartening to know that my grandmother could have lived longer and suffered less if available technologies had been used to provide continuous healthcare, and not just acute sick care. Technology solutions are readily available to help provide continuous care for those living with chronic conditions. We don’t have to wait for the next doctor visit to understand when something might become a problem. Insight into what is happening in our lives every day, outside of the healthcare setting, is vital to improving health. Now we in healthcare need to harness and use that data to more effectively care for patients with chronic disease.